Skin&lab Dr Vita Clinic Fre-c Sun Protector Review
| Skin | |
|---|---|
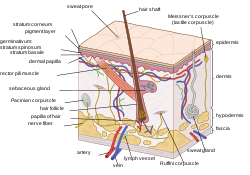 Epidermis, dermis, and subcutis, showing a hair follicle, gland, and sebaceous gland | |
| Details | |
| System | Integumentary system |
| Identifiers | |
| Latin | cutis |
| MeSH | D012867 |
| TA98 | A16.0.00.002 |
| TA2 | 7041 |
| Th | H3.12.00.1.00001 |
| FMA | 7163 |
| Anatomical terminology [edit on Wikidata] | |
The human skin is the outer covering of the body and is the largest organ of the integumentary arrangement. The skin has upwards to seven layers of ectodermal tissue guarding muscles, bones, ligaments and internal organs. Human skin is similar to most of the other mammals' skin, and it is very similar to sus scrofa peel. Though nigh all human skin is covered with hair follicles, it can announced hairless. In that location are two general types of peel, hairy and glabrous pare (hairless). The describing word cutaneous literally means "of the peel" (from Latin cutis, pare).
Because information technology interfaces with the environment, pare plays an important immunity role in protecting the body against pathogens and excessive water loss. Its other functions are insulation, temperature regulation, awareness, synthesis of vitamin D, and the protection of vitamin B folates. Severely damaged peel will try to heal by forming scar tissue. This is frequently discoloured and depigmented.
In humans, pare pigmentation (afflicted by melanin) varies among populations, and skin type can range from dry to non-dry and from oily to non-oily. Such skin variety provides a rich and diverse habitat for leaner that number roughly 1000 species from nineteen phyla, present on the human skin.
Structure [edit]
Human skin shares anatomical, physiological, biochemical and immunological properties with other mammalian lines, especially pig pare.[ane] [2] Pig skin shares similar epidermal and dermal thickness ratios to human skin;[1] [2] pig and human skin share similar hair follicle and blood vessel patterns;[1] [2] biochemically the dermal collagen and elastic content is similar in grunter and human skin;[i] [two] and pig peel and human skin have like physical responses to various growth factors.[1] [two]
Skin has mesodermal cells, pigmentation, such as melanin provided by melanocytes, which absorb some of the potentially dangerous ultraviolet radiation (UV) in sunlight. It besides contains DNA repair enzymes that help contrary UV damage, such that people lacking the genes for these enzymes suffer high rates of skin cancer. One class predominantly produced by UV light, malignant melanoma, is particularly invasive, causing it to spread quickly, and can often be mortiferous. Human skin pigmentation varies amidst populations in a striking manner. This has led to the classification of people(due south) on the basis of skin colour.[three]
In terms of surface area, the skin is the second largest organ in the human body (the inside of the pocket-size intestine is 15 to 20 times larger). For the boilerplate developed human, the skin has a surface area of from 1.5–2.0 square metres (16–22 sq ft). The thickness of the skin varies considerably over all parts of the body, and betwixt men and women and the young and the old. An instance is the pare on the forearm which is on average 1.iii mm in the male and 1.26 mm in the female person.[four] One average foursquare inch (half dozen.5 cmii) of skin holds 650 sweat glands, xx blood vessels, 60,000 melanocytes, and more than 1,000 nerve endings.[5] [ better source needed ] The average human skin jail cell is nigh 30 micrometres (μm) in diameter, but there are variants. A skin jail cell normally ranges from 25–40 μm2, depending on a multifariousness of factors.
Skin is equanimous of 3 primary layers: the epidermis, the dermis and the hypodermis.[4]

Layers, Receptors, and Appendages of Human being Peel
Epidermis [edit]
Epidermis, "epi" coming from the Greek meaning "over" or "upon", is the outermost layer of the skin. Information technology forms the waterproof, protective wrap over the torso'southward surface which also serves as a barrier to infection and is fabricated up of stratified squamous epithelium with an underlying basal lamina.
The epidermis contains no claret vessels, and cells in the deepest layers are nourished most exclusively by diffused oxygen from the surrounding air[6] and to a far bottom degree past blood capillaries extending to the outer layers of the dermis. The main type of cells that brand upwards the epidermis are Merkel cells, keratinocytes, with melanocytes and Langerhans cells also nowadays. The epidermis tin can be further subdivided into the following strata (beginning with the outermost layer): corneum, lucidum (only in palms of easily and bottoms of feet), granulosum, spinosum, and basale. Cells are formed through mitosis at the basale layer. The daughter cells (see cell division) move up the strata irresolute shape and composition as they die due to isolation from their claret source. The cytoplasm is released and the protein keratin is inserted. They eventually reach the corneum and slough off (desquamation). This process is chosen "keratinization". This keratinized layer of peel is responsible for keeping water in the body and keeping other harmful chemicals and pathogens out, making skin a natural bulwark to infection.[7]

2d project of a 3D October-tomogram of the pare at the fingertip, depicting the stratum corneum (~500 µm thick) with the stratum disjunctum on top and the stratum lucidum in the centre. At the lesser are the superficial parts of the dermis. The sweat ducts are conspicuously visible. (See also: Rotating 3D Version)
The epidermis contains no blood vessels and is nourished by diffusion from the dermis. The main type of cells that brand up the epidermis are keratinocytes, melanocytes, Langerhans cells, and Merkel cells. The epidermis helps the skin regulate body temperature.
Layers [edit]
The pare has up to vii layers of ectodermal tissue and guards the underlying muscles, basic, ligaments and internal organs.[8] The epidermis is divided into several layers, where cells are formed through mitosis at the innermost layers. They motility up the strata changing shape and composition as they differentiate and become filled with keratin. After reaching the top layer stratum corneum they are eventually 'sloughed off', or desquamated. This process is called keratinization and takes identify within weeks.
It was previously believed that the stratum corneum was "a elementary, biologically inactive, outer epidermal layer comprising a fibrillar lattice of dead keratin".[nine] It is at present understood that this is not true, and that the stratum corneum should be considered to exist a live tissue.[10] While information technology is truthful that the stratum corneum is mainly composed of terminally differentiated keratinocytes chosen corneocytes that are anucleated, these cells remain alive and metabolically functional until desquamated.[ citation needed ]
Sublayers [edit]
The epidermis is divided into the post-obit v sublayers or strata:
- Stratum corneum
- Stratum lucidum
- Stratum granulosum
- Stratum spinosum
- Stratum basale (likewise called "stratum germinativum")
Blood capillaries are plant below the epidermis and are linked to an arteriole and a venule. Arterial shunt vessels may bypass the network in ears, the nose and fingertips.
Genes and proteins expressed in the epidermis [edit]
About 70% of all human protein-coding genes are expressed in the skin.[11] [12] Almost 500 genes have an elevated blueprint of expression in the skin. There are less than 100 genes that are specific for the skin, and these are expressed in the epidermis.[xiii] An analysis of the corresponding proteins show that these are mainly expressed in keratinocytes and have functions related to squamous differentiation and cornification.
Dermis [edit]
The dermis is the layer of skin beneath the epidermis that consists of connective tissue and cushions the body from stress and strain. The dermis is tightly continued to the epidermis past a basement membrane. It also harbours many nervus endings that provide the sense of touch and heat. Information technology contains the hair follicles, sweat glands, sebaceous glands, apocrine glands, lymphatic vessels and blood vessels. The blood vessels in the dermis provide nourishment and waste product removal from its ain cells as well equally from the stratum basale of the epidermis.
The dermis is structurally divided into 2 areas: a superficial area adjacent to the epidermis, called the papillary region, and a deep thicker expanse known as the reticular region.
Papillary region [edit]
The papillary region is composed of loose areolar connective tissue. It is named for its finger-like projections called papillae, which extend toward the epidermis. The papillae provide the dermis with a "bumpy" surface that interdigitates with the epidermis, strengthening the connectedness betwixt the two layers of pare.
In the palms, fingers, soles, and toes, the influence of the papillae projecting into the epidermis forms contours in the skin's surface. These epidermal ridges occur in patterns (run into: fingerprint) that are genetically and epigenetically determined and are therefore unique to the individual, making it possible to apply fingerprints or footprints as a means of identification.
Reticular region [edit]
The reticular region lies deep in the papillary region and is usually much thicker. Information technology is composed of dense irregular connective tissue, and receives its name from the dense concentration of collagenous, elastic, and reticular fibres that weave throughout information technology. These protein fibres requite the dermis its backdrop of strength, extensibility, and elasticity.
Also located within the reticular region are the roots of the hairs, sebaceous glands, sweat glands, receptors, nails, and claret vessels.
Tattoo ink is held in the dermis. Stretch marks, often from pregnancy and obesity, are besides located in the dermis.
Subcutaneous tissue [edit]
The subcutaneous tissue (likewise hypodermis and subcutis) is not part of the skin, only lies beneath the dermis of the cutis. Its purpose is to attach the peel to underlying bone and musculus as well as supplying it with claret vessels and nerves. It consists of loose connective tissue, adipose tissue and elastin. The main cell types are fibroblasts, macrophages and adipocytes (subcutaneous tissue contains 50% of trunk fatty). Fat serves every bit padding and insulation for the body.
Cross-section [edit]
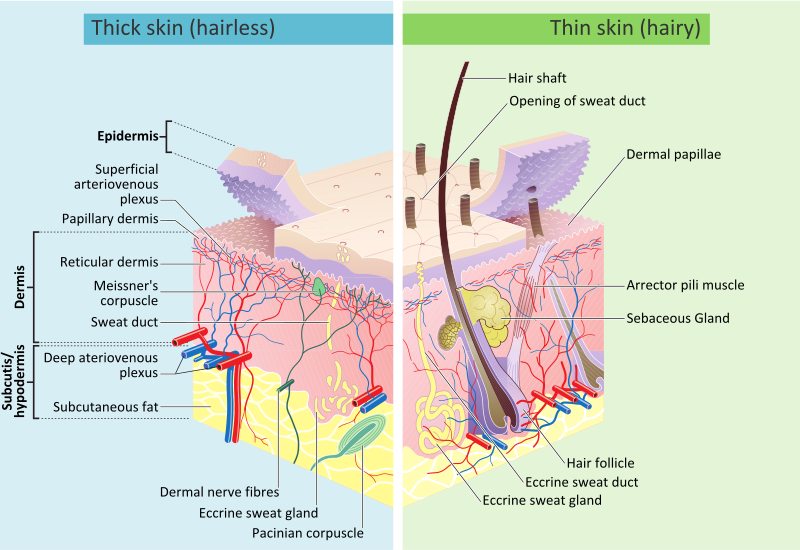
Skin layers, of both hairy and hairless skin
Development [edit]
Skin colour [edit]
Human being peel shows high skin color variety from the darkest brown to the lightest pink-white hues. Human skin shows higher variation in color than whatever other single mammalian species and is the result of natural selection. Skin pigmentation in humans evolved to primarily regulate the corporeality of ultraviolet radiation (UVR) penetrating the pare, controlling its biochemical effects.[14]
The bodily skin colour of different humans is affected past many substances, although the single most important substance determining human pare colour is the pigment melanin. Melanin is produced inside the skin in cells chosen melanocytes and it is the master determinant of the peel colour of darker-skinned humans. The skin colour of people with light skin is determined mainly by the bluish-white connective tissue under the dermis and by the haemoglobin circulating in the veins of the dermis. The reddish color underlying the skin becomes more visible, especially in the confront, when, as consequence of concrete exercise or the stimulation of the nervous system (anger, fright), arterioles amplify.[xv]
In that location are at least v different pigments that determine the colour of the peel.[16] [17] These pigments are nowadays at different levels and places.
- Melanin: Information technology is brown in colour and present in the basal layer of the epidermis.
- Melanoid: It resembles melanin just is present diffusely throughout the epidermis.
- Carotene: This pigment is yellow to orange in color. Information technology is nowadays in the stratum corneum and fat cells of dermis and superficial fascia.
- Hemoglobin (also spelled haemoglobin): It is institute in claret and is non a pigment of the skin but develops a purple color.
- Oxyhemoglobin: Information technology is too plant in blood and is not a pigment of the skin. It develops a red color.
There is a correlation between the geographic distribution of UV radiations (UVR) and the distribution of indigenous pare pigmentation around the globe. Areas that highlight college amounts of UVR reflect darker-skinned populations, more often than not located nearer towards the equator. Areas that are far from the tropics and closer to the poles have lower concentration of UVR, which is reflected in lighter-skinned populations.[18]
In the same population it has been observed that developed human being females are considerably lighter in peel pigmentation than males. Females need more calcium during pregnancy and lactation, and vitamin D which is synthesized from sunlight helps in absorbing calcium. For this reason it is thought that females may have evolved to accept lighter skin in order to assist their bodies absorb more than calcium.[19]
The Fitzpatrick scale[twenty] [21] is a numerical classification schema for man skin colour developed in 1975 as a manner to classify the typical response of different types of skin to ultraviolet (UV) light:
| I | Always burns, never tans | Pale, Off-white, Freckles |
| Ii | Usually burns, sometimes tans | Fair |
| III | May burn down, ordinarily tans | Calorie-free Brown |
| IV | Rarely burns, always tans | Olive brown |
| V | Moderate ramble pigmentation | Chocolate-brown |
| VI | Marked constitutional pigmentation | Blackness |
Ageing [edit]


Every bit skin ages, it becomes thinner and more easily damaged. Intensifying this issue is the decreasing ability of pare to heal itself as a person ages.
Among other things, pare ageing is noted by a decrease in book and elasticity. In that location are many internal and external causes to pare ageing. For instance, ageing peel receives less claret flow and lower glandular activity.
A validated comprehensive grading calibration has categorized the clinical findings of pare ageing as laxity (sagging), rhytids (wrinkles), and the diverse facets of photoageing, including erythema (redness), and telangiectasia, dyspigmentation (brownish discolouration), solar elastosis (yellowing), keratoses (abnormal growths) and poor texture.[22]
Cortisol causes degradation of collagen,[23] accelerating skin ageing.[24]
Anti-ageing supplements are used to treat pare ageing.[ citation needed ]
Photoageing [edit]
Photoageing has two main concerns: an increased take a chance for peel cancer and the appearance of damaged peel. In younger skin, sun harm will heal faster since the cells in the epidermis accept a faster turnover rate, while in the older population the skin becomes thinner and the epidermis turnover rate for cell repair is lower, which may upshot in the dermis layer beingness damaged.[25]
Types [edit]
| | This section needs expansion. You lot can help by calculation to it. (March 2022) |
Though nigh human skin is covered with hair follicles, some parts can be hairless. There are two full general types of skin, hairy and glabrous skin (hairless).[26] The describing word cutaneous means "of the skin" (from Latin cutis, peel).[27]
Functions [edit]
Pare performs the post-obit functions:
- Protection: an anatomical barrier from pathogens and damage between the internal and external environment in bodily defence; Langerhans cells in the skin are part of the adaptive immune organization.[seven] [28] Perspiration contains lysozyme that break the bonds inside the cell walls of bacteria.[29]
- Sensation: contains a diversity of nerve endings that react to estrus and cold, touch, force per unit area, vibration, and tissue injury; run across somatosensory system and haptics.
- Heat regulation: the pare contains a blood supply far greater than its requirements which allows precise control of energy loss past radiation, convection and conduction. Dilated claret vessels increase perfusion and oestrus loss, while constricted vessels greatly reduce cutaneous claret flow and conserve heat.
- Command of evaporation: the peel provides a relatively dry and semi-impermeable barrier to fluid loss.[28] Loss of this role contributes to the massive fluid loss in burns.
- Aesthetics and communication: others meet our skin and can appraise our mood, physical state and bewitchery.
- Storage and synthesis: acts as a storage center for lipids and water, as well as a ways of synthesis of vitamin D by activeness of UV on certain parts of the skin.
- Excretion: sweat contains urea, however its concentration is i/130th that of urine, hence excretion by sweating is at about a secondary role to temperature regulation.
- Assimilation: the cells comprising the outermost 0.25–0.twoscore mm of the pare are "almost exclusively supplied past external oxygen", although the "contribution to total respiration is negligible".[6] In addition, medicine can be administered through the skin, by ointments or past means of adhesive patch, such as the nicotine patch or iontophoresis. The peel is an important site of transport in many other organisms.
- H2o resistance: The skin acts as a h2o-resistant barrier so essential nutrients are non washed out of the body.[28]
Skin flora [edit]
The human skin is a rich environment for microbes.[xxx] [31] Around 1000 species of bacteria from 19 bacterial phyla have been found.[31] [30] Most come from only four phyla: Actinomycetota (51.viii%), Bacillota (24.4%), Pseudomonadota (16.5%), and Bacteroidota (6.3%). Propionibacteria and Staphylococci species were the main species in sebaceous areas. There are three main ecological areas: moist, dry and sebaceous. In moist places on the body Corynebacteria together with Staphylococci boss. In dry areas, there is a mixture of species simply dominated by Betaproteobacteria and Flavobacteriales. Ecologically, sebaceous areas had greater species richness than moist and dry ones. The areas with least similarity between people in species were the spaces between fingers, the spaces between toes, axillae, and umbilical cord stump. Most similarly were beside the nostril, nares (inside the nostril), and on the dorsum.
Reflecting upon the diversity of the man skin researchers on the human skin microbiome have observed: "hairy, moist underarms prevarication a short altitude from smooth dry forearms, just these two niches are likely as ecologically different as rainforests are to deserts."[30]
The NIH conducted the Human Microbiome Project to narrate the human being microbiota which includes that on the peel and the role of this microbiome in wellness and illness.[32]
Microorganisms like Staphylococcus epidermidis colonize the skin surface. The density of skin flora depends on region of the skin. The disinfected pare surface gets recolonized from leaner residing in the deeper areas of the pilus follicle, gut and urogenital openings.
Clinical significance [edit]
Diseases of the skin include skin infections and peel neoplasms (including skin cancer). Dermatology is the branch of medicine that deals with conditions of the skin.[26]
The skin is also valuable for diagnosis of other conditions, since many medical signs show through the pare. Skin color affects the visibility of these signs, a source of misdiagnosis in unaware medical personnel.[33] [34]
Society and civilization [edit]
Hygiene and pare care [edit]
The pare supports its own ecosystems of microorganisms, including yeasts and bacteria, which cannot be removed by any amount of cleaning. Estimates place the number of individual bacteria on the surface of six.5 square centimetres (1 sq in) of human skin at fifty million, though this figure varies greatly over the average 1.9 square metres (twenty sq ft) of human skin. Oily surfaces, such as the face, may contain over 78 million leaner per square centimetre (500 one thousand thousand per foursquare inch). Despite these vast quantities, all of the bacteria constitute on the pare'southward surface would fit into a volume the size of a pea.[35] In general, the microorganisms keep one another in check and are part of a healthy skin. When the balance is disturbed, there may exist an overgrowth and infection, such equally when antibiotics kill microbes, resulting in an overgrowth of yeast. The peel is continuous with the inner epithelial lining of the body at the orifices, each of which supports its own complement of microbes.
Cosmetics should be used carefully on the pare considering these may cause allergic reactions. Each flavour requires suitable habiliment in order to facilitate the evaporation of the sweat. Sunlight, water and air play an important role in keeping the skin salubrious.
Oily pare [edit]
Oily skin is caused by over-active sebaceous glands, that produce a substance chosen sebum, a naturally healthy pare lubricant.[8] [36] A high glycemic-index diet and dairy products (except for cheese) consumption increase IGF-1 generation, which in turn increases sebum production.[36] Overwashing the skin does not cause sebum overproduction but may cause dryness.[36]
When the peel produces excessive sebum, information technology becomes heavy and thick in texture, known equally oily skin.[36] Oily peel is typified past shininess, blemishes and pimples.[8] The oily-peel type is not necessarily bad, since such pare is less prone to wrinkling, or other signs of ageing,[8] because the oil helps to keep needed moisture locked into the epidermis (outermost layer of peel). The negative aspect of the oily-pare type is that oily complexions are especially susceptible to clogged pores, blackheads, and buildup of expressionless peel cells on the surface of the skin.[8] Oily pare can be sallow and rough in texture and tends to have large, clearly visible pores everywhere, except around the eyes and neck.[8]
Permeability [edit]
Human skin has a depression permeability; that is, virtually foreign substances are unable to penetrate and diffuse through the skin. Skin's outermost layer, the stratum corneum, is an effective barrier to virtually inorganic nanosized particles.[37] [38] This protects the trunk from external particles such as toxins past not assuasive them to come into contact with internal tissues. However, in some cases it is desirable to allow particles entry to the trunk through the skin. Potential medical applications of such particle transfer has prompted developments in nanomedicine and biology to increase skin permeability. One awarding of transcutaneous particle delivery could be to locate and care for cancer. Nanomedical researchers seek to target the epidermis and other layers of agile cell partitioning where nanoparticles can interact direct with cells that have lost their growth-control mechanisms (cancer cells). Such direct interaction could be used to more than accurately diagnose properties of specific tumours or to care for them by delivering drugs with cellular specificity.
Nanoparticles [edit]
Nanoparticles forty nm in diameter and smaller accept been successful in penetrating the skin.[39] [40] [41] Inquiry confirms that nanoparticles larger than 40 nm do not penetrate the skin past the stratum corneum.[39] Most particles that practise penetrate will diffuse through skin cells, but some will travel downwards hair follicles and reach the dermis layer.
The permeability of peel relative to different shapes of nanoparticles has also been studied. Inquiry has shown that spherical particles have a better ability to penetrate the pare compared to oblong (oblong) particles because spheres are symmetric in all three spatial dimensions.[41] 1 study compared the 2 shapes and recorded information that showed spherical particles located deep in the epidermis and dermis whereas ellipsoidal particles were mainly found in the stratum corneum and epidermal layers.[42] Nanorods are used in experiments because of their unique fluorescent backdrop but have shown mediocre penetration.
Nanoparticles of different materials have shown skin's permeability limitations. In many experiments, gilded nanoparticles 40 nm in diameter or smaller are used and have shown to penetrate to the epidermis. Titanium oxide (TiO2), zinc oxide (ZnO), and argent nanoparticles are ineffective in penetrating the peel by the stratum corneum.[38] [43] Cadmium selenide (CdSe) quantum dots accept proven to penetrate very effectively when they have sure properties. Because CdSe is toxic to living organisms, the particle must be covered in a surface group. An experiment comparing the permeability of quantum dots coated in polyethylene glycol (PEG), PEG-amine, and carboxylic acrid concluded the PEG and PEG-amine surface groups allowed for the greatest penetration of particles. The carboxylic acid coated particles did non penetrate past the stratum corneum.[42]
Increasing permeability [edit]
Scientists previously believed that the pare was an effective bulwark to inorganic particles. Impairment from mechanical stressors was believed to be the only way to increase its permeability.[44]
Recently, simpler and more effective methods for increasing skin permeability have been adult. Ultraviolet radiation (UVR) slightly damages the surface of skin and causes a time-dependent defect allowing easier penetration of nanoparticles.[45] The UVR's high energy causes a restructuring of cells, weakening the boundary between the stratum corneum and the epidermal layer.[45] [44] The damage of the skin is typically measured by the transepidermal water loss (TEWL), though it may have 3–5 days for the TEWL to reach its top value. When the TEWL reaches its highest value, the maximum density of nanoparticles is able to permeate the peel. While the issue of increased permeability later UVR exposure can pb to an increment in the number of particles that permeate the skin, the specific permeability of skin later UVR exposure relative to particles of different sizes and materials has not been adamant.[45]
There are other methods to increase nanoparticle penetration by skin damage: tape stripping is the process in which tape is applied to skin so lifted to remove the tiptop layer of skin; peel abrasion is done past shaving the top 5–10 μm off the surface of the skin; chemical enhancement applies chemicals such as polyvinylpyrrolidone (PVP), dimethyl sulfoxide (DMSO), and oleic acid to the surface of the skin to increase permeability;[46] [47] electroporation increases skin permeability by the application of brusk pulses of electric fields. The pulses are high voltage and on the gild of milliseconds when applied. Charged molecules penetrate the peel more than frequently than neutral molecules after the pare has been exposed to electrical field pulses. Results have shown molecules on the lodge of 100 μm to easily permeate electroporated skin.[47]
Applications [edit]
A large area of interest in nanomedicine is the transdermal patch because of the possibility of a painless application of therapeutic agents with very few side effects. Transdermal patches have been limited to administrate a pocket-sized number of drugs, such as nicotine, considering of the limitations in permeability of the skin. Development of techniques that increase skin permeability has led to more drugs that can be applied via transdermal patches and more than options for patients.[47]
Increasing the permeability of skin allows nanoparticles to penetrate and target cancer cells. Nanoparticles forth with multi-modal imaging techniques have been used every bit a way to diagnose cancer non-invasively. Skin with high permeability allowed quantum dots with an antibiotic fastened to the surface for agile targeting to successfully penetrate and identify cancerous tumours in mice. Tumour targeting is benign because the particles can be excited using fluorescence microscopy and emit light energy and rut that will destroy cancer cells.[48]
Sunblock and sunscreen [edit]
Sunblock and sunscreen are different of import skin-intendance products though both offer full protection from the sun.[49] [50]
Sunblock—Sunblock is opaque and stronger than sunscreen, since information technology is able to block most of the UVA/UVB rays and radiation from the sun, and does non need to be reapplied several times in a day. Titanium dioxide and zinc oxide are two of the important ingredients in sunblock.[51]
Sunscreen—Sunscreen is more than transparent once applied to the peel and too has the ability to protect against UVA/UVB rays, although the sunscreen'south ingredients have the power to interruption downwards at a faster charge per unit in one case exposed to sunlight, and some of the radiation is able to penetrate to the skin. In order for sunscreen to exist more effective it is necessary to consistently reapply and use one with a college sunday protection factor.
Diet [edit]
Vitamin A, likewise known every bit retinoids, benefits the skin by normalizing keratinization, downregulating sebum production which contributes to acne, and reversing and treating photodamage, striae, and cellulite.
Vitamin D and analogues are used to downregulate the cutaneous immune system and epithelial proliferation while promoting differentiation.
Vitamin C is an antioxidant that regulates collagen synthesis, forms barrier lipids, regenerates vitamin E, and provides photoprotection.
Vitamin East is a membrane antioxidant that protects confronting oxidative damage and also provides protection against harmful UV rays. [52]
Several scientific studies confirmed that changes in baseline nutritional status affects skin status. [53]
The Mayo Clinic lists foods they state help the peel: fruits and vegetables, whole-grains, nighttime leafy greens, nuts, and seeds.[54]
See likewise [edit]
- Acid mantle
- Anthropodermic bibliopegy
- Artificial peel
- Callus, thick area of skin
- Listing of cutaneous conditions
- Cutaneous structure development
- Fingerprint, peel on fingertips
- Hyperpigmentation, about backlog skin color
- Intertriginous
- Meissner'due south corpuscle
- Pacinian corpuscle
- Polyphenol antioxidant
- Peel cancer
- Skin lesion
- Skin repair
References [edit]
- ^ a b c d e Herron AJ (5 December 2009). "Pigs as Dermatologic Models of Homo Skin Illness" (PDF). ivis.org. DVM Center for Comparative Medicine and Department of Pathology Baylor College of Medicine Houston, Texas. Retrieved 27 January 2018.
sus scrofa skin has been shown to be the nigh similar to human skin. Pig skin is structurally like to human epidermal thickness and dermal-epidermal thickness ratios. Pigs and humans have like pilus follicle and blood vessel patterns in the skin. Biochemically pigs contain dermal collagen and elastic content that is more similar to humans than other laboratory animals. Finally pigs have like concrete and molecular responses to various growth factors.
- ^ a b c d due east Liu J, Kim D, Chocolate-brown L, Madsen T, Bouchard GF. "Comparing of Human being, Porcine and Rodent Wound Healing With New Miniature Swine Written report Data" (PDF). sinclairresearch.com. Sinclair Enquiry Centre, Auxvasse, MO, USA; Veterinary Medical Diagnostic Laboratory, Columbia, MO, USA. Retrieved 27 January 2018.
Sus scrofa pare is anatomically, physiologically, biochemically and immunologically like to human being peel
- ^ Maton A, Hopkins J, McLaughlin CW, Johnson S, Warner MQ, LaHart D, Wright JD (1893). Man Biological science and Health . Englewood Cliffs, New Jersey, USA: Prentice Hall. ISBN978-0-thirteen-981176-0.
- ^ a b Wilkinson PF, Millington R (2009). Peel (Digitally printed version ed.). Cambridge: Cambridge University Printing. pp. 49–50. ISBN978-0-521-10681-8.
- ^ Bennett H (25 May 2014). "Ever wondered about your skin?". The Washington Post . Retrieved 27 October 2014.
- ^ a b Stücker M, Struk A, Altmeyer P, Herde M, Baumgärtl H, Lübbers DW (February 2002). "The cutaneous uptake of atmospheric oxygen contributes significantly to the oxygen supply of human being dermis and epidermis". The Journal of Physiology. 538 (Pt 3): 985–94. doi:10.1113/jphysiol.2001.013067. PMC2290093. PMID 11826181.
- ^ a b Proksch E, Brandner JM, Jensen JM (December 2008). "The pare: an indispensable barrier". Experimental Dermatology. 17 (12): 1063–72. doi:10.1111/j.1600-0625.2008.00786.10. PMID 19043850. S2CID 31353914.
- ^ a b c d due east f "Skin care" (analysis), Health-Cares.internet, 2007, webpage: HCcare Archived 12 Dec 2007 at the Wayback Machine
- ^ Del Rosso JQ, Levin J (September 2011). "The clinical relevance of maintaining the functional integrity of the stratum corneum in both healthy and disease-afflicted pare". The Periodical of Clinical and Aesthetic Dermatology. iv (9): 22–42. doi:10.1111/j.1365-2133.1990.tb06268.x. PMC3175800. PMID 21938268.
- ^ Kligman A (2006). "A brief history of how the dead stratum corneum became alive". Skin Barrier. New York: Taylor & Francis. pp. 35–44. ISBN9780429163470.
- ^ "The man proteome in peel – The Human Protein Atlas". www.proteinatlas.org.
- ^ Uhlén M, Fagerberg L, Hallström BM, Lindskog C, Oksvold P, Mardinoglu A, et al. (Jan 2015). "Proteomics. Tissue-based map of the human proteome". Science. 347 (6220): 1260419. doi:x.1126/science.1260419. PMID 25613900. S2CID 802377.
- ^ Edqvist PH, Fagerberg Fifty, Hallström BM, Danielsson A, Edlund K, Uhlén Thou, Pontén F (Feb 2015). "Expression of human being skin-specific genes defined by transcriptomics and antibiotic-based profiling". The Journal of Histochemistry and Cytochemistry. 63 (two): 129–41. doi:10.1369/0022155414562646. PMC4305515. PMID 25411189.
- ^ Muehlenbein Grand (2010). Human Evolutionary Biology. Cambridge Academy Press. pp. 192–213. ISBN978-1139789004.
- ^ Jablonski NG (2006). Skin: a Natural History . Berkeley: University of California Press. ISBN978-0520954816.
- ^ Handbook of General Beefcake by B. D. Chaurasia. ISBN 978-81-239-1654-5
- ^ "Pigmentation of Skin". Mananatomy.com. Archived from the original on 7 Oct 2012. Retrieved 3 June 2019.
- ^ Webb AR (September 2006). "Who, what, where and when-influences on cutaneous vitamin D synthesis". Progress in Biophysics and Molecular Biology. 92 (1): 17–25. doi:10.1016/j.pbiomolbio.2006.02.004. PMID 16766240.
- ^ Jablonski NG, Chaplin Thousand (July 2000). "The evolution of human skin coloration". Journal of Human Evolution. 39 (1): 57–106. doi:10.1006/jhev.2000.0403. PMID 10896812.
- ^ "The Fitzpatrick Peel Type Classification Scale". Skin Inc. (November 2007). 28 May 2009. Retrieved 7 January 2014.
- ^ "Fitzpatrick Peel Type" (PDF). Australian Radiation Protection and Nuclear Rubber Agency. Archived from the original (PDF) on 31 March 2016. Retrieved 7 January 2014.
- ^ Alexiades-Armenakas, One thousand. R., et al. The spectrum of laser peel resurfacing: nonablative, fractional, and ablative laser resurfacing. J Am Acad Dermatol. 2008 May;58(5):719-37; quiz 738-40
- ^ Cutroneo KR, Sterling KM (May 2004). "How practise glucocorticoids compare to oligo decoys equally inhibitors of collagen synthesis and potential toxicity of these therapeutics?". Journal of Cellular Biochemistry. 92 (1): 6–15. doi:10.1002/jcb.20030. PMID 15095399. S2CID 24160757. (subscription required)
- ^ Oikarinen A (2004). "Connective tissue and crumbling". International Periodical of Corrective Science. 26 (2): 107. doi:10.1111/j.1467-2494.2004.213_6.x. ISSN 0142-5463. (subscription required)
- ^ Gilchrest BA (April 1990). "Skin aging and photoaging". Dermatology Nursing. 2 (2): 79–82. PMID 2141531.
- ^ a b Marks, James G; Miller, Jeffery (2006). Lookingbill and Marks' Principles of Dermatology. (quaternary ed.). Elsevier Inc. ISBN 1-4160-3185-five.
- ^ "Definition of CUTANEOUS". world wide web.merriam-webster.com . Retrieved iv March 2022.
- ^ a b c Madison KC (Baronial 2003). "Bulwark part of the skin: "la raison d'être" of the epidermis" (PDF). The Periodical of Investigative Dermatology. 121 (two): 231–41. doi:10.1046/j.1523-1747.2003.12359.x. PMID 12880413.
- ^ Todar K. "Immune Defence force against Bacterial Pathogens: Innate Immunity". textbookofbacteriology.cyberspace . Retrieved nineteen April 2017.
- ^ a b c Grice EA, Kong HH, Conlan Southward, Deming CB, Davis J, Young AC, et al. (May 2009). "Topographical and temporal diverseness of the human pare microbiome". Science. 324 (5931): 1190–2. Bibcode:2009Sci...324.1190G. doi:x.1126/science.1171700. PMC2805064. PMID 19478181.
- ^ a b Pappas Southward. (2009). Your Body Is a Wonderland ... of Bacteria. ScienceNOW Daily News Archived 2 June 2009 at the Wayback Motorcar
- ^ "NIH Homo Microbiome Project". Hmpdacc.org. Retrieved iii June 2019.
- ^ "Color awareness: A must for patient assessment". American Nurse. 11 January 2011.
- ^ McCue D (21 July 2020). "Medical student creates handbook for diagnosing conditions in Black and dark-brown skin". As It Happens. CBC Radio. Retrieved 15 December 2020.
- ^ Theodor Rosebury. Life on Man: Secker & Warburg, 1969 ISBN 0-670-42793-4
- ^ a b c d Sakuma Th, Maibach Hullo (2012). "Oily skin: an overview". Pare Pharmacology and Physiology. 25 (5): 227–35. doi:10.1159/000338978. PMID 22722766. S2CID 2446947.
- ^ Baroli B (Jan 2010). "Penetration of nanoparticles and nanomaterials in the skin: fiction or reality?". Journal of Pharmaceutical Sciences. 99 (1): 21–50. doi:10.1002/jps.21817. PMID 19670463.
- ^ a b Filipe P, Silva JN, Silva R, Cirne de Castro JL, Marques Gomes M, Alves LC, et al. (2009). "Stratum corneum is an effective barrier to TiOtwo and ZnO nanoparticle percutaneous absorption". Skin Pharmacology and Physiology. 22 (5): 266–75. doi:x.1159/000235554. PMID 19690452. S2CID 25769287.
- ^ a b Vogt A, Combadiere B, Hadam Southward, Stieler KM, Lademann J, Schaefer H, et al. (June 2006). "xl nm, only not 750 or 1,500 nm, nanoparticles enter epidermal CD1a+ cells after transcutaneous application on human pare". The Journal of Investigative Dermatology. 126 (half-dozen): 1316–22. doi:10.1038/sj.jid.5700226. PMID 16614727.
- ^ a b Ryman-Rasmussen JP, Riviere JE, Monteiro-Riviere NA (May 2006). "Penetration of intact skin by quantum dots with various physicochemical backdrop". Toxicological Sciences. 91 (1): 159–65. doi:ten.1093/toxsci/kfj122. PMID 16443688.
- ^ a b Ryman-Rasmussen, J.P., Riviere, J.E. and Monteiro-Riviere, N.A. Penetration of Intact Skin by Breakthrough Dots with Diverse Physicochemical Properties. Toxicological Sciences 2006;91(1):159–165
- ^ Larese FF, D'Agostin F, Crosera K, Adami G, Renzi North, Bovenzi M, Maina 1000 (January 2009). "Human being pare penetration of silver nanoparticles through intact and damaged skin". Toxicology. 255 (one–two): 33–vii. doi:ten.1016/j.tox.2008.09.025. PMID 18973786.
- ^ a b Mortensen LJ, Oberdörster Chiliad, Pentland AP, Delouise LA (September 2008). "In vivo skin penetration of quantum dot nanoparticles in the murine model: the effect of UVR". Nano Letters. 8 (nine): 2779–87. Bibcode:2008NanoL...8.2779M. doi:10.1021/nl801323y. PMC4111258. PMID 18687009.
- ^ a b c Mortensen L, Zheng H, Faulknor R, De Benedetto A, Beck L, DeLouise LA (2009). Osinski M, Jovin TM, Yamamoto Thou (eds.). "Increased in vivo skin penetration of quantum dots with UVR and in vitro breakthrough dot cytotoxicity". Colloidal Quantum Dots for Biomedical Applications IV. 7189: 718919–718919–12. Bibcode:2009SPIE.7189E..19M. doi:10.1117/12.809215. ISSN 0277-786X. S2CID 137060184.
- ^ Sokolov K, Follen Chiliad, Aaron J, Pavlova I, Malpica A, Lotan R, Richards-Kortum R (May 2003). "Real-time vital optical imaging of precancer using anti-epidermal growth factor receptor antibodies conjugated to gold nanoparticles". Cancer Inquiry. 63 (ix): 1999–2004. PMID 12727808.
- ^ a b c Prausnitz MR, Mitragotri South, Langer R (February 2004). "Current status and hereafter potential of transdermal drug delivery". Nature Reviews. Drug Discovery. 3 (2): 115–24. doi:x.1038/nrd1304. PMID 15040576. S2CID 28888964.
- ^ Gao X, Cui Y, Levenson RM, Chung LW, Nie S (August 2004). "In vivo cancer targeting and imaging with semiconductor quantum dots". Nature Biotechnology. 22 (eight): 969–76. doi:10.1038/nbt994. PMID 15258594. S2CID 41561027.
- ^ "Sunscreen or sunblock". Retrieved 1 July 2015.
- ^ An update on Suncreens; 2007; P 23- 29. Bachelor at www.aocd.org/resources/resmgr/jaocd/2007aug.pdf
- ^ "Nanotechnology Data Center: Properties, Applications, Research, and Rubber Guidelines". American Elements.
- ^ Shapiro SS, Saliou C (October 2001). "Role of vitamins in skin intendance". Nutrition. 17 (10): 839–44. doi:10.1016/S0899-9007(01)00660-viii. PMID 11684391.
- ^ Boelsma Eastward, van de Vijver LP, Goldbohm RA, Klöpping-Ketelaars IA, Hendriks HF, Roza 50 (February 2003). "Man skin condition and its associations with food concentrations in serum and nutrition". The American Journal of Clinical Nutrition. 77 (2): 348–55. doi:10.1093/ajcn/77.2.348. PMID 12540393.
- ^ "Foods for healthy skin". Mayo Clinic.
External links [edit]
| | Look up homo skin in Wiktionary, the free dictionary. |
-
 Media related to Human skin at Wikimedia Commons
Media related to Human skin at Wikimedia Commons - MedlinePlus Skin Weather condition National Library of Medicine retrieved 12 November 2013.
Source: https://en.wikipedia.org/wiki/Human_skin
0 Response to "Skin&lab Dr Vita Clinic Fre-c Sun Protector Review"
Post a Comment